Bipolar Disorder: Symptoms, Causes, Types, and Treatment
Bipolar disorder is a complex mood condition characterized by dramatic swings in energy, activity levels, and emotional states, manifesting as periods of elevated mood (mania or hypomania) alternating with depressive episodes. Understanding the symptoms of bipolar disorder is essential for recognizing when professional intervention is needed.
During manic episodes, individuals may experience an abnormally elevated or irritable mood, coupled with a surge in energy that often leads to decreased need for sleep, rapid or pressured speech, racing thoughts, distractibility, grandiose beliefs, and impulsive behaviors, sometimes escalating to risky activities or psychotic features in severe cases. Hypomanic episodes share many of these qualities but are milder in intensity and shorter in duration, allowing for some preserved functioning despite noticeable behavioral changes.
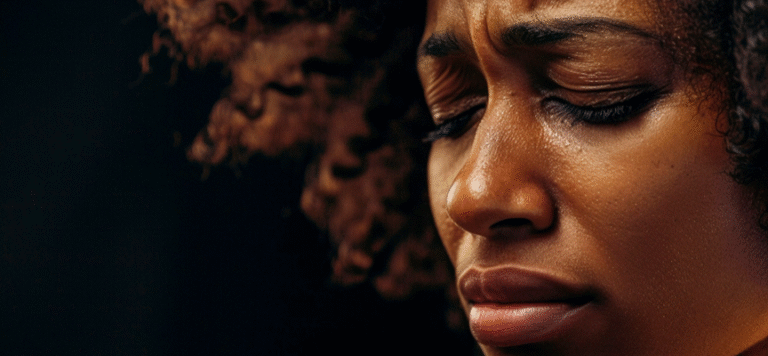
Conversely, the depressive phases of bipolar disorder involve prolonged periods of sadness or hopelessness, loss of interest in once-enjoyed activities, fatigue, significant changes in appetite or sleep patterns, difficulty concentrating, and recurrent thoughts of death or suicide. Additionally, mixed features can occur when symptoms of both mania and depression co-occur, placing individuals at heightened risk for self-harm. Cognitive impairments, particularly in areas like memory, attention, and executive function, can persist between mood episodes, further impacting daily performance and quality of life.
While the causes of bipolar disorder are not fully understood, research consistently points to a multifactorial etiology in which genetic, biological, and environmental factors intersect. A strong genetic component is evident, with heritability estimates ranging as high as 70–80 %, and first-degree relatives of affected individuals face significantly increased risk. Neurobiological studies reveal structural brain differences, including variations in cortical thickness and subcortical volumes tied to mood regulation circuits, alongside dysregulation of key neurotransmitters such as dopamine and serotonin. Yet genes alone do not dictate destiny; stressful life events, such as traumatic experiences, significant losses, relationship breakdowns, or chronic stress, can precipitate or intensify mood episodes, particularly in those with underlying vulnerability. Substance misuse, including alcohol and recreational drugs, further compounds risk by destabilizing mood and interfering with treatment adherence. Ultimately, bipolar disorder emerges from a dynamic interplay of inherited predispositions, neurochemical imbalances, and psychosocial stressors, underscoring the need for a holistic approach to both understanding and addressing the condition.
The effects of bipolar disorder extend far beyond the immediate experience of mood swings, casting a wide shadow over social, occupational, medical, and psychological domains. Functionally, mood episodes can disrupt work performance, academic pursuits, and everyday responsibilities, while interpersonal relationships often strain under the weight of unpredictable behavior and communication challenges. Even in remission, many individuals contend with lingering cognitive difficulties, such as problems with planning, decision-making, and memory, that hinder full participation in social and professional life. Physically, people with bipolar disorder exhibit elevated rates of comorbid medical conditions including obesity, metabolic syndrome, type 2 diabetes, cardiovascular disease, migraine, and thyroid dysfunction. These health issues not only decrease life expectancy, on average by a decade, but also complicate psychiatric treatment and heighten overall disease burden. Perhaps most alarmingly, the risk of suicide among those with bipolar disorder is markedly increased: estimates indicate that roughly one-third of affected individuals attempt suicide at least once, with 15–20 % dying by suicide. Mixed mood states and severe depressive episodes confer especially high risk, demanding vigilant monitoring and rapid intervention.
Compounding these challenges, possible comorbidities of bipolar disorder are both diverse and prevalent, often obscuring diagnosis and complicating management. Anxiety disorders, including generalized anxiety, panic disorder, and obsessive-compulsive disorder, co-occur in approximately 70 % of cases, amplifying distress and functional impairment. Substance use disorders, particularly involving alcohol or illicit drugs, afflict around half of individuals with bipolar disorder, exacerbating mood instability and undermining treatment efficacy. Coexisting personality disorders, most commonly borderline or antisocial types, are observed in roughly one-third of patients, further complicating emotional regulation and interpersonal relationships. Attention‑deficit/hyperactivity disorder appears in 10–20 % of cases, and post-traumatic stress disorder frequently overlaps with bipolar symptoms, sharing features of hyperarousal, emotional dysregulation, and impulsivity. Medical comorbidities compound the psychiatric picture: metabolic and cardiovascular conditions, in particular, are more common in bipolar populations, necessitating integrated care strategies that address both mental and physical health.
Effectively managing bipolar disorder demands a comprehensive, individualized plan encompassing pharmacological, psychotherapeutic, and lifestyle interventions. Medications remain the cornerstone of treatment: mood stabilizers such as lithium are recognized for reducing the frequency and severity of both manic and depressive episodes and for lowering suicide risk, though they require regular blood monitoring due to narrow therapeutic margins and potential kidney or thyroid effects. Anticonvulsants, including valproate and carbamazepine, serve as alternatives for acute mania or rapid cycling, while lamotrigine demonstrates particular efficacy in preventing depressive relapses. Atypical antipsychotics, such as quetiapine and olanzapine, are employed for mania or mixed states and sometimes improve depressive symptoms. Antidepressants are used cautiously, and typically only in conjunction with a mood stabilizer, to avoid triggering manic switches or rapid mood fluctuations.
Beyond medication, psychotherapy plays a vital role. Cognitive Behavioral Therapy (CBT) targets distorted beliefs and unhealthy behavior patterns to bolster coping skills; Family-Focused Therapy fosters a supportive environment through improved communication and shared problem-solving; Interpersonal and Social Rhythm Therapy (IPSRT) emphasizes stabilizing daily routines, such as consistent sleep, meal, and activity schedules, to regulate circadian rhythms and reduce relapse risk. Psychoeducation helps individuals and families recognize early warning signs and adhere to treatment plans.
In addition, structured lifestyle and self‑management strategies reinforce medical and psychotherapeutic efforts. Regular exercise promotes mood stability and overall health; mindfulness and stress reduction techniques mitigate the impact of external pressures; adherence to sleep hygiene principles safeguards against destabilizing fatigue or insomnia; and involvement in peer support networks cultivates understanding and resilience. Monitoring comorbid medical conditions, through routine screenings for metabolic indicators, cardiovascular risk factors, and thyroid function, is equally essential to comprehensive care. Best outcomes arise when treatment teams integrate psychiatric, psychological, and primary care providers, collaborating across disciplines to tailor interventions to each person’s symptom profile, comorbidities, and life circumstances.
Ultimately, living with bipolar disorder is an ongoing journey that encompasses more than just symptom control. Recognizing the symptoms of bipolar disorder, understanding its causes, and acknowledging the broad effects of bipolar disorder lay the groundwork for timely diagnosis and early intervention. Addressing the possible comorbid conditions of bipolar disorder through vigilant assessment prevents misdiagnosis and unplanned treatment complications. And implementing evidence‑based approaches in the management of bipolar disorder, from medications to therapy, lifestyle adjustments to integrated medical care, enables individuals to achieve stability, reduce relapse rates, and pursue fulfilling lives.
By framing bipolar disorder as a treatable, manageable condition rather than an insurmountable barrier, we shift the narrative toward empowerment and recovery. With compassionate support, tailored interventions, and an emphasis on strengths as well as vulnerabilities, those affected by bipolar disorder can harness opportunities for growth and transformation, cultivating resilience that extends beyond symptom remission to the creation of richer, purpose-driven lives.